Testicular cancer is the most commonly diagnosed cancer in men aged 15 to 29 years. The incidence of this condition has increased gradually over the last few decades. In addition, this form of cancer seems more common in Caucasian men compared to those of African origin.
In most cases, the discovery of testicular cancer is by self-examination of the testes, usually after trauma or stroke to the genital area.
There are two types of testicular cancer: seminoma (30%) and non-seminoma (70%).
Causes Testicular cancer
The cause of testicular cancer is still unknown. Here are some risk factors for this disease:
•a family history of testicular cancer;
•a personal history of testicular cancer;
•smoking;
•cryptorchidism (undescended testes).
Some studies suggest that infertility is a risk factor for testicular cancer, but this is not proven. There is no association between testicular cancer and vasectomy, diet or trauma.
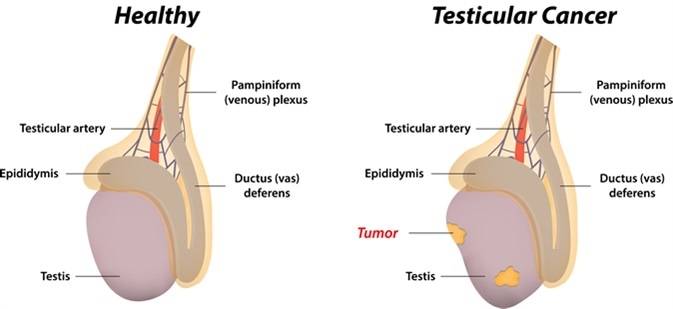
Symptoms and Complications of Testicular cancer
The symptoms of testicular cancer include:
•the presence of a painless mass in the testicle (common);
•a dull pain in the groin or abdomen (uncommon)
•enlargement of the testicle (frequent);
•pain, discomfort or "heaviness" in the scrotum (bursae) (uncommon)
•pain or discomfort in the testis (uncommon)
Occasionally, the symptoms come from the spread of the disease to another organ, such as bumps in the neck, a cough due to the presence of cancer in the lungs, back pain caused by the presence of cancer in the bones and, in rare cases, neurological problems.
Treatment of testicular cancer can lead to various complications. Radiation therapy can cause erectile dysfunction (eg, getting and maintaining an erection), while chemotherapy is associated with a risk of infertility.
In addition, men who have had testicular cancer appear to be at higher risk for leukemia and other cancers.
Diagnostic of Testicular cancer
There is no evidence to support the adoption of a monthly self-testicle test. However, such an examination can help you and your doctor detect abnormal changes sooner. If you decide to examine yourself, the best time is after a bath or a shower, and the best place is in front of a mirror.
To do this, take a testicle in your hands and feel the different parts by gently rolling each testicle between thumb and forefinger, looking for anomalies or bumps. Repeat the process for the other testicle. You should recognize the oval shape of the testicles, which are smooth and firm. Check for lump around the epididymis, the duct at the top and back of the testicle.
When a patient has a suspicious testicular tumor, the doctor checks his family history, performs a complete physical examination, including testes and scrotum, and requests blood tests. Blood tests will measure the levels of chemical markers that may indicate the presence of cancer. Then the doctor can prescribe an ultrasound of the scrotum, an examination that can detect masses or abnormalities in the testicles.
The next diagnostic step is the biopsy of the tumor. It is an intervention that involves removing the affected testicle (excision-biopsy) and examining the tissue for evidence of cancer. Although this is the excision of the whole testicle, the operation is not done through the scrotum but rather using an incision in the groin. Removing the entire testicle reduces the risk of cancer spreading.
The chemical markers of the tumor found in the blood can be very useful for the diagnosis of testicular cancer as well as for its treatment and follow-up. The mode of appearance of these markers (alpha-fetoprotein, human beta chorionic gonadotropin and lactic dehydrogenase) may help determine the type of testicular cancer and the type of treatment indicated.
Once the diagnosis is made, it is important to determine the stage of the cancer. This is done by performing a chest X-ray and CT scan or magnetic resonance imaging of the abdomen and pelvic area, as well as bone scans. The X-ray shows whether the cancer has invaded the lungs, while the CT scan shows how it spreads to the lymph nodes of the abdomen. Some doctors recommend the use of special contrast media in X-rays. Thus, intravenous pyelographyallows the urinary tract to be explored, and lymphangiography is used to visualize the lymphatic system.
Here are the different stages of testicular cancer:
•stage 1: the cancer is still limited to the testis or the level of at least one tumor marker is very high;
•stage 2: the cancer has spread to the abdominal lymph nodes;
•Stage 3: The cancer has spread to other parts of the body, such as the lungs or liver, or the cancer has spread to the lymph nodes of the abdomen and the tumor marker levels are high.
Treatment and Prevention of Testicular cancer
The first-line treatment for testicular cancer is surgery, which aims to excise the affected testicle. A testicular implant may be placed for aesthetic reasons. With the remaining testicle, the person being treated can still have children and normal erections.
The surgical procedure may be followed by radiation therapy, chemotherapy or a combination of both. For some people, no treatment is recommended after surgery. However, the therapeutic team will follow you regularly. The oncologist (a doctor who specializes in cancer treatment) often recommends follow-up after surgery, based on the type of cancer and the stage of the disease.
Early stage seminomas are often treated with a combination of surgery and radiotherapy or chemotherapy. Non-seminomatous germ cell tumors are often treated with larger surgical procedures such as radical retroperitoneallymphadenectomy (removal of some lymph nodes in the back of the abdomen) followed by vigilant surveillance or chemotherapy. Often, the use of chemotherapy or surgery depends on the estimated risk of cancer worsening or spread (mild, intermediate or high). Various factors, such as the type and stage of cancer, and general health status, may indicate that one treatment is more appropriate than another.
For more advanced disease, such as bulky tumors or metastatic disease, chemotherapeutic treatment may still be very effective. There is still a significant rate of cure even for testicular cancer that has spread to other parts of the body. Sometimes, for a high-risk disease, but especially for recurrent cancer, high-dose chemotherapy with autologous stem cell input (a bone marrow transplant from the patient's own stem cells after high-dose chemotherapy) allows for long-term remission or even cure.
Side effects of radiotherapy include:
•loss of appetite
•diarrhea;
•fatigue
•nausea
•redness and dryness of the skin at the point of irradiation.
Radiation therapy can reduce fertility, but sperm production should recover over time.
As chemotherapy drugs circulate throughout the body, more systems or organs are affected by the treatment. Side effects of chemotherapy include:
•chills;
•diarrhea;
•fatigue
•hair loss
•lesions in the mouth;
•nausea and vomiting
•shortness of breath
Some forms of chemotherapy can cause infertility; you must therefore discuss this question before the start of treatment. Also, it is recommended to discuss it beforehand, and people who wish to procreate later should see with their doctor the possibility of storing their sperm.
After cancer treatment, physicians usually recommend that patients undergo blood tests and chest X-rays every month for one year, and every 2 months during the second year to ensure the efficacy of the treatment and treatment. Prolonged absence of cancer.
Men with testicular cancer are likely to feel particularly vulnerable psychologically, especially because this cancer strikes them in years when they could start a family. Good psychological support is an important part of the healing process as a whole.
In general, testicular cancer has a favorable outcome: the earlier the screening, the better the result. Cancer may, however, reappear; also, those who have received treatment should watch for signs of a return of cancer. According to statistics, it is during the first year after treatment that the probability of recurrence of cancer is highest.